MIT spinout Sigilon Therapeutics has partnered with pharmaceutical giant Eli Lilly and Company to develop implantable medical devices that act like “living drug factories,” encapsulating engineered cells that live in the body for months, or years, and produce insulin. Down the road, cells may also be engineered to secrete other hormones, proteins, and antibodies.
By implanting “living drug factories” into the bodies of diabetes patients, researchers believe they could eliminate the everyday hassle of finger pricks and insulin injections.
Sigilon Therapeutics—a company that originated from research conducted at the Massachusetts Institute of Technology and Harvard Medical School—is developing an implantable, insulin-producing device that could replace the constant need for insulin injections to control the disease. They are working with pharmaceutical company Eli Lilly and Company.
Following a minimally invasive procedure, a device comprised of tiny hydrogel beads that encases the cells and protects them from the individual patient’s immune system, is placed in a patient’s body.
The new implant is comprised of encapsulated, engineered cells that produce insulin over the course of months or years.
“This allows us to have ‘living drug factories’ inside our bodies that can deliver therapeutics, at the right amount and in the right location, as needed,” co-founder and co-inventor Daniel Anderson, an associate professor in MIT’s Department of Chemical Engineering, Institute for Medical Engineering and Science, and Koch Institute for Integrative Cancer Research, said in a statement. “The hope is that this living device can be placed in a patient, avoid the need for immune-suppression, and provide long-term therapy.”
Most diabetics have to prick their fingers several times a day to draw blood and test blood-sugar levels. They are then forced to inject themselves with insulin when it is necessary.
While effective, the treatment is often dosed incorrectly, leading to uncontrolled blood sugar levels.
Cell therapy, where patients receive transplanted human cells that secrete a protein, hormone or other agents to fight the disease, also can be used to combat diabetes.
Patients with diabetes receive transplanted pancreatic beta cells, from cadavers, which sense blood sugar levels and produce insulin in response.
While this treatment results in the long-term control of blood-sugar levels and makes insulin injections obsolete, it often forces patients to take immune suppressants or their immune systems will reject and kill the foreign cells.
Researchers have recently began to focus on cell encapsulation—surrounding transplanted cells in a thin polymer film to stave off the immune response, while still nourishing the cells. While the therapies have shown potential to treat several diseases like cancer, heart failure, hemophilia, glaucoma and Parkinson’s disease, the treatment has not yet made it to the market.
More than 10 years ago, researchers began to look at developing new technological approaches toward islet cell encapsulation. However, it proved to be a challenge to identify the right material that protected cells but also was essentially invisibly to the immune system.
The majority of the materials placed in the body led to scar tissue accumulation through a process called fibrosis. When medical devices are covered in scar tissue they become isolated from the body, which can block transfer of insulin and cause encapsulated cells to die.
To overcome this obstacle, the researchers combined chemically modified alginate—a polysaccharide that lines the cell walls of brown algae with water to produce a gel that can safely encapsulate cells without limiting function. To ensure that the coating would not cause fibrosis, the researchers attached different molecules to the alginate’s polymer chain, chemically modifying the structure hundreds of times until they found the version that did not provoke an immune response.
“A hydrogel that keeps cells alive and is permeable so that sugar and nutrients can come in and insulin can come out, but still blocks cellular elements of the immune system, like T cells, which can destroy the therapeutic cells inside,” Anderson said.
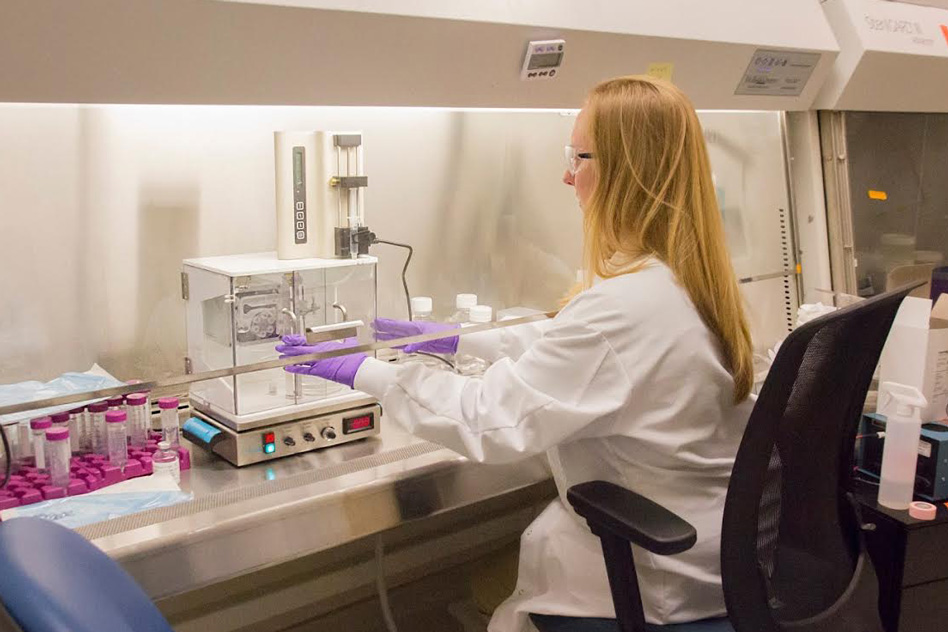
To test this, the researchers implanted cells encapsulated in their hydrogel into animals and found that the cells immediately produced therapeutic amounts of insulin in response to blood sugar levels. The treatment also kept blood sugar levels under control over the duration of the six-month study and that small capsules of the hydrogel implanted in the patients—which did not contain engineered cells—prevented fibrosis.
“There had been a growing collection of scientific work, taking different approaches to this problem,” Anderson said. “The key challenge was finding materials that avoid scar tissue formation.”