Researchers may have found a better way to understand the dormant form of a parasite that leads to malaria and is resistant to most antimalarial drugs.
Researchers from the Massachusetts Institute of Technology have developed a way to grow the dormant parasite in engineered human liver tissue for several weeks, allowing them to closely study how the parasite becomes dormant, what vulnerabilities it may have and how it can reawaken months or years later, causing disease relapse.
The researchers successfully cultivated the dormant form of the parasite and found that they could sequence its RNA. They also were able to test its response to known and novel antimalarial drugs, which could led to the eventual eradication of the disease.
“After 10 years of hard work, we were able to grow the organism, show it had all the functional hallmarks, perform a drug screen against it, and report the first transcriptome of this elusive form,” Sangeeta Bhatia, the John and Dorothy Wilson Professor of Health Sciences and Technology and Electrical Engineering and Computer Science, said in a statement. “I’m really excited because I believe it will open the door to both the basic biology of dormancy as well as the possibility of better medicines.”
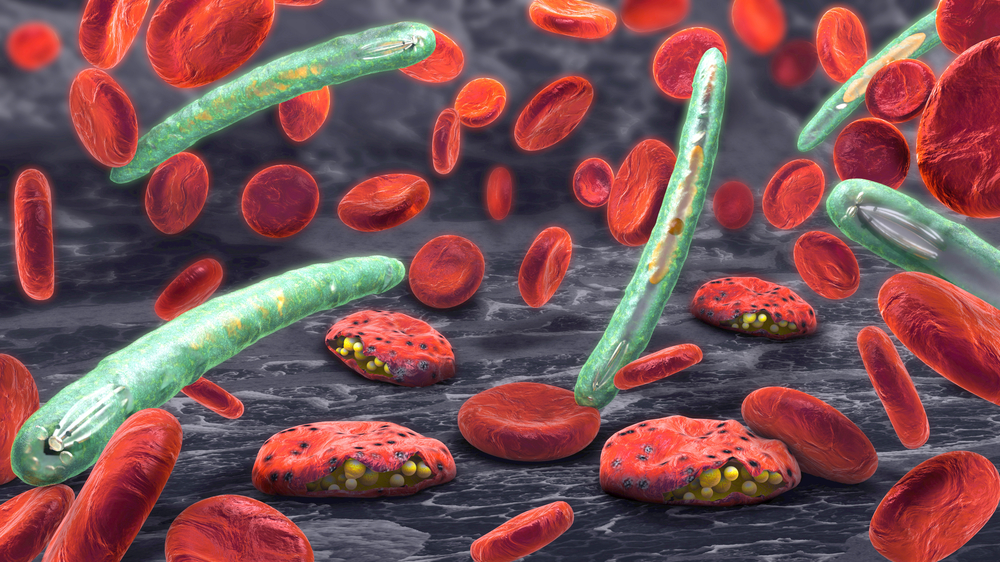
The majority of malaria cases in humans are caused by either parasite species Plasmodium falciparum or Plasmodium vivax, which produces dormant forms called hypnozoites and can lead to recurring infections.
“This dormant form has been seen as the critical barrier to eradication,” Bhatia said. “You can treat the symptoms of vivax malaria by killing all the parasites in the blood, but if hypnozoites linger in someone’s liver, these forms can reactivate and reinfect the blood of a patient.
“If a mosquito comes along and takes a blood meal, the cycle starts all over again,” she added. “So, if we want to eradicate malaria, we have to eradicate the hypnozoite.”
The only drug that can fight off hypnozoites is primaquine. However, the drug cannot be used in large-scale eradication campaigns because it causes blood cells to rupture in people with a certain enzyme deficiency.
The researchers were able to grow small forms of the parasite that had all the known features of hypnozoites—persistence, sensitivity to primaquine and the ability to reoccur after a few weeks.
The researchers then obtained six candidate antimalarials now in development and tested them for activity against their Plasmodium vivax samples. None of the candidates could kill the established hypnozoites.
They now plan to test a larger set of new compounds and plan to use single cell RNA-sequencing to identify gene signatures to uncover the signaling pathways that control hypnozoite dormancy and reactivation.
They also plan to study the corresponding changes in gene expression of the infected liver cells, which could yield potential new drug candidates that would specifically target the dormant forms of the parasite.
In 2015, it was estimated that malaria infected more than 200 million people and killed an estimated 429,000.




