Using
state-of-the-art technology, scientists at The University of Nottingham have discovered a new class of
polymers that are resistant to
bacterial attachment. These new materials could lead to a significant reduction
in hospital infections and medical device failures.
Medical device
associated infections can lead to systemic infections or device failure.
Affecting many commonly used devices including urinary and venous catheters—bacteria form communities known as biofilms. This strength-in-numbers approach
protects them against the bodies’ natural defenses and antibiotics.
Experts in the Schools
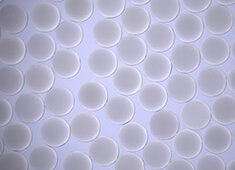
of Pharmacy and Molecular Medical Sciences, have shown that when the new materials are applied to the surface of
medical devices they repel bacteria and prevent them forming biofilms.
The research was
led by Professor Morgan Alexander, and Professor Martyn Davies in the School of
Pharmacy and Professor Paul Williams in the School of Molecular Medical Sciences.
The results of the four-year research project supported by a Translation Award
from the Wellcome Trust, have
been published in Nature Biotechnology.
The novel
materials had to be found using a new technique
Researchers believed there were new materials that could resist bacteria better
but they had to find them. This meant screening thousands of different
chemistries and testing their reaction to bacteria—a challenge which was beyond
conventional materials development or any of our current understanding of the
interaction of microorganisms with surfaces.
The discovery has
been made with the help of experts from the Massachusetts Institute of Technology
(MIT)—who initially developed the process by which thousands of unique polymers
can now be screened simultaneously.
Alexander said: “This is a major scientific breakthrough—we have discovered a new group of
structurally related materials that dramatically reduce the attachment of
pathogenic bacteria (Pseudomonas aeruginosa, Staphylococcus aureus, and Escherichia
coli). We could not have found these materials using the current
understanding of bacteria-surface interactions. The technology developed with
the help of MIT means that hundreds of materials could be screened
simultaneously to reveal new structure-property relationships. In total
thousands of materials were investigated using this high-throughput materials
discovery approach leading to the identification of novel materials resisting
bacterial attachment. This could not have been achieved using conventional
techniques.”
These new
materials prevent infection by stopping biofilm formation at the earliest possible
stage—when the bacteria first attempt to attach themselves to the device. In
the laboratory experts were able to reduce the numbers of bacteria by up to 96.7%—compared
with a commercially available silver containing catheter—and were effective at
resisting bacterial attachment in a mouse implant infection model. By
preventing bacterial attachment the body’s own immune system can kill the
bacteria before they have time to generate biofilms.
Ted Bianco,
director of technology transfer at the Wellcome Trust, said: “Infections caused
by microbial biofilms binding to the surface of implants often cannot be
treated with conventional antibiotics. This makes them a significant challenge
in patient care, particularly for those with inserted medical devices like
catheters, heart valves, and prosthetic joints. The discovery of these new
polymers is a great example of how advances in materials science are being
exploited in our efforts to improve the performance of critical medical
components. Just as materials science gave us the non-stick saucepan, so
we look forward to the day of the ‘non-stick’ medical device.”
Bacterial attachment
and subsequent biofilm formation are key challenges to the performance of
medical devices. This is early-stage research but the initial results are very
promising. The next stage of this research will be to develop the manufacture
of these coatings to enable the performance of these materials to be assessed
clinically and the inventors are in early stage discussions with a number of medical
device companies.
Source: The University of Nottingham