Researchers have developed a new method in predicting whether high-risk infants will eventually develop autism.
A new diagnostic method has correctly predicted autism in 80 percent of high-risk infants, according to a new study.
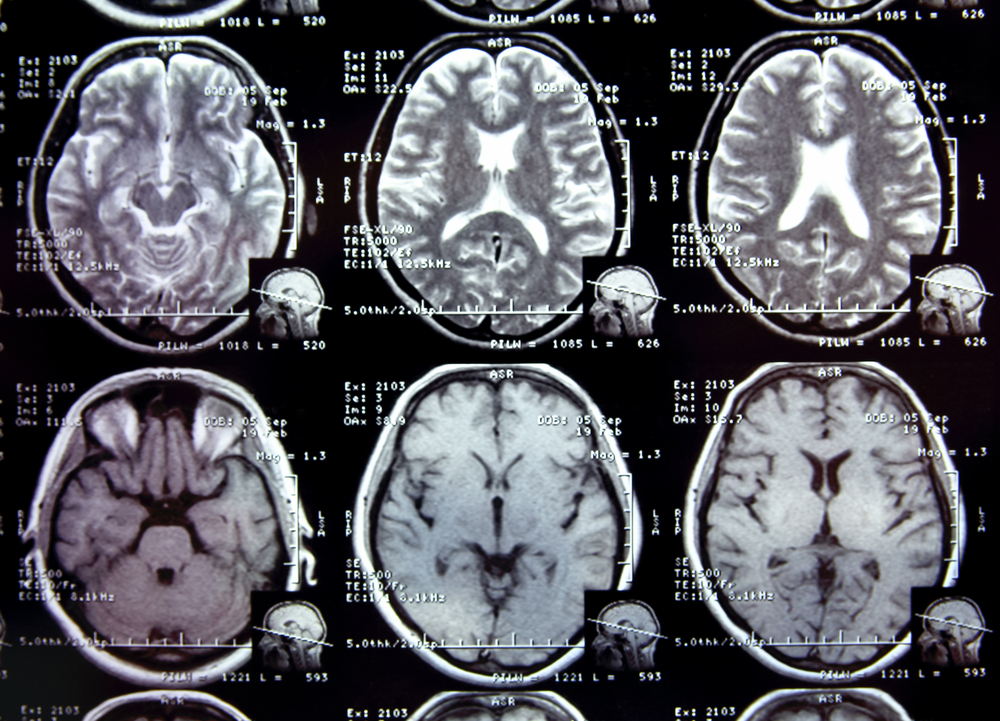
Researchers at the University of North Carolina have developed a method using magnetic resonance imaging (MRI) in infants with older siblings with autism to correctly predict whether infants would later meet the criteria for autism at two years old.
“Our study shows that early brain development biomarkers could be very useful in identifying babies at the highest risk for autism before behavioral symptoms emerge,” Dr. Joseph Piven, the Thomas E. Castelloe Distinguished Professor of Psychiatry at UNC and senior author of the paper, said in a statement. “Typically, the earliest an autism diagnosis can be made is between ages two and three. But for babies with older autistic siblings, our imaging approach may help predict during the first year of life which babies are most likely to receive an autism diagnosis at 24 months.”
It is estimated that one out of every 68 children develop Autism Spectrum Disorder (ASD) in the U.S. The patients have characteristic social deficits and demonstrate a range of ritualistic, repetitive and stereotyped behaviors.
Despite extensive research, it has been impossible to identify those at ultra-high risk for autism prior to two-years old, which is the earliest time when the hallmark behavioral characteristics of ASD can be observed and a diagnosis made in most children.
In the study, the researchers conducted MRI scans of infants at six, 12 and 24 months old.
The researchers found that the babies who developed autism experienced a hyper-expansion of brain surface area from six to 12 months, as compared to babies who had an older sibling with autism but did not themselves show evidence of the condition at 24 months of age.
They also found that increased growth rate of surface area in the first year of life was linked to increased growth rate of overall brain volume in the second year, which is tied to the emergence of autistic social deficits in the second year.
The next step was to take the data—MRI’s of brain volume, surface area, cortical thickness at six and 12 months of age and the sex of the infants—and used a computer program to identify a way to classify babies most likely to meet criteria for autism at two-years old.
The computer program developed an algorithm that the researchers applied to a separate set of study participants.
The researchers concluded that brain differences at six and 12 months in infants with older siblings with autism correctly predicted eight of 10 infants who would later meet criteria for autism at two-years old in comparison to those with older ASD siblings who did not meet the criteria at two years old.
“This means we potentially can identify infants who will later develop autism, before the symptoms of autism begin to consolidate into a diagnosis,” Piven said.
This test could be helpful to parents who have a child with autism and have a second child, where they could intervene ‘pre-symptomatically’ before the emergence of the defining symptoms of autism.
Researchers could then begin to examine the effect of interventions on children during a period before the syndrome is present and when the brain is most malleable.
“Putting this into the larger context of neuroscience research and treatment, there is currently a big push within the field of neurodegenerative diseases to be able to detect the biomarkers of these conditions before patients are diagnosed, at a time when preventive efforts are possible,” Piven said. “In Parkinson’s for instance, we know that once a person is diagnosed, they’ve already lost a substantial portion of the dopamine receptors in their brain, making treatment less effective.”
The research, which was led by researchers at the Carolina Institute for Developmental Disabilities (CIDD) at the University of North Carolina, where Piven is director, included hundreds of children from across the country.
The project’s other clinical sites included the University of Washington, Washington University in St. Louis and The Children’s Hospital of Philadelphia. Other key collaborators are McGill University, the University of Alberta, the University of Minnesota, the College of Charleston and New York University.
“This study could not have been completed without a major commitment from these families, many of whom flew in to be part of this,” first author Heather Hazlett, Ph.D., assistant professor of psychiatry at the UNC School of Medicine and a CIDD researcher, said in a statement.




