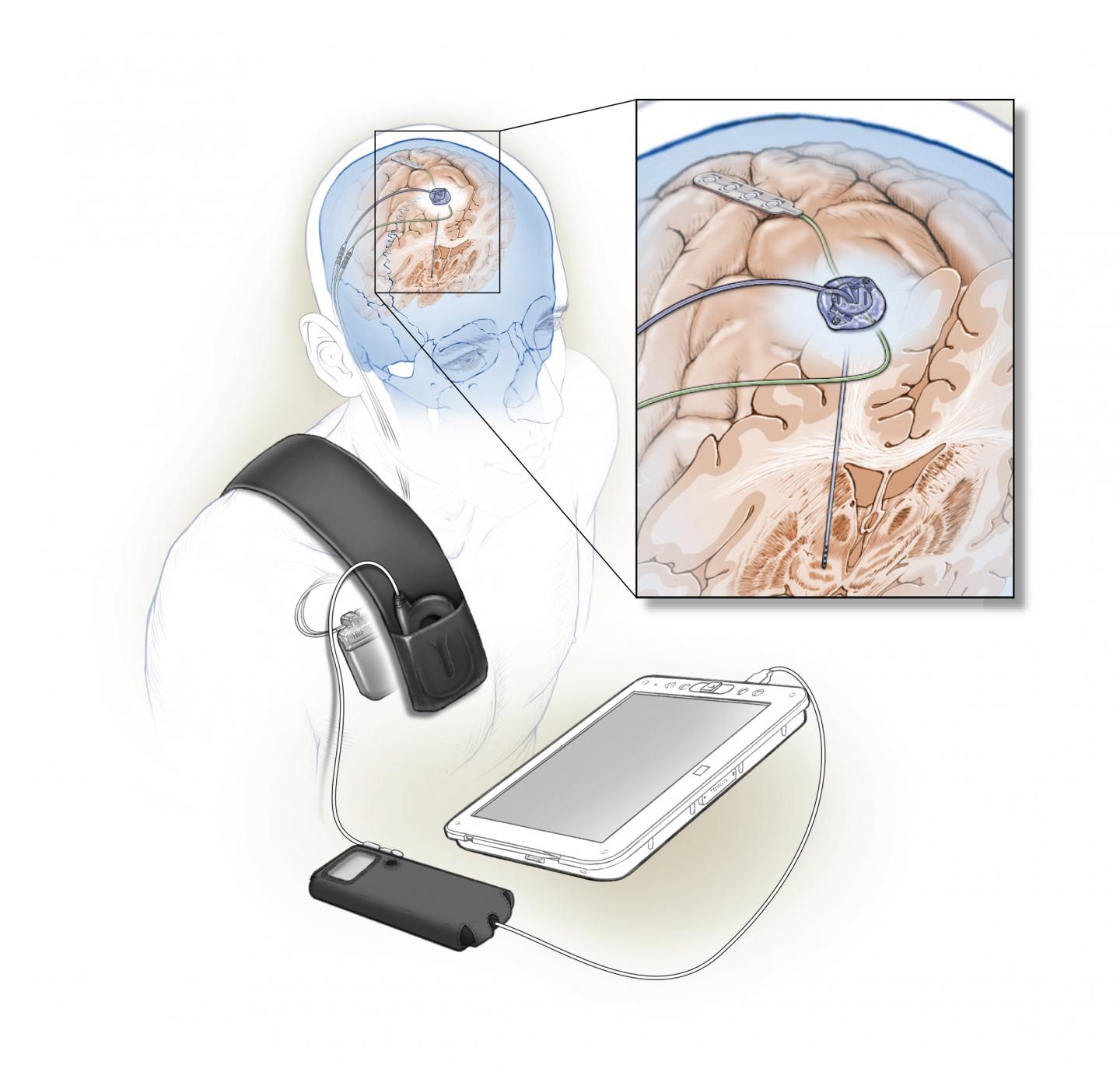
Stimulating and sensing electrodes are implanted in the brain and connect to small computer under the skin. Data from this computer can be read by an external device.
A team of researchers has improved on the deep brain stimulation technique that has been used to treat Parkinson’s disease for the last 25 years.
Researchers from the National Institute of Neurological Disorders and Stroke (NINDS) have developed a fully implanted deep brain stimulation system that uses feedback from the brain to fine-tune its signaling and eliminate some of the side effects that plague traditional deep brain stimulation.
“The novel approach taken in this small-scale feasibility study may be an important first step in developing a more refined or personalized way for doctors to reduce the problems patients with Parkinson’s disease face every day,” Nick Langhals, PhD, program director at NINDS and team lead for the BRAIN Initiative, said in a statement.
In deep brain stimulation, an electrode is surgically implanted into the brain to deliver constant stimulation to a part of the brain called the basal ganglia to help treat the symptoms of Parkinson’s. While it effectively treats the symptoms, it can lead to unwanted side effects that require reprogramming by trained clinicians.
However, the new method is adaptive, so the stimulation delivered is responsive in real time to signals received from the patient’s brain.
“This is the first time a fully implanted device has been used for closed-loop, adaptive deep brain stimulation in human Parkinson’s disease patients,” Philip Starr, MD, PhD, professor of neurological surgery, University of California, San Francisco, and senior author of the study, said in a statement.
In a short-term feasibility trial, two patients with Parkinson’s received a fully implanted, adaptive deep brain stimulation device that can monitor and modulate brain activity. The sensing was done from an electrode implanted over the primary motor cortex—the part of the brain critical for normal movement.
Signals from the electrode are then fed into a computer program embedded in the device to determine whether to stimulate the brain.
The researchers taught the program to recognize a pattern of brain activity associated with dyskinesia, or uncontrolled movements—a side effect of deep brain stimulation in Parkinson’s disease—as a guide to tailor stimulation.
The stimulation was reduced when it identified dyskinesia-related brain activity and increased when brain sensing found no dyskinesia to minimize deep brain stimulation-related side effects.
The researchers sought to demonstrate the feasibility and effectiveness of using adaptive deep brain stimulation to overcome the impediment to movement of Parkinson’s. The results suggest that the adaptive approach was equally effective at controlling symptoms as traditional deep brain stimulation.
The short time periods over which movement was assessed did not permit comparison of the two deep brain stimulation paradigms relative to incidence of dyskinesia. However, the researchers hope that the variable stimulation will also translate into a reduction in adverse effects when tested over a long period.
“Other adaptive deep brain stimulation designs record brain activity from an area adjacent to where the stimulation occurs, in the basal ganglia, which is susceptible to interference from stimulation current,” Starr said. “Instead, our device receives feedback from the motor cortex, far from the stimulation source, providing a more reliable signal.
“Here we have demonstrated the feasibility of adaptive deep brain stimulation,” he added. “We are now planning larger, longer-term trials to determine how effective this system is in managing the symptoms of patients with Parkinson’s disease.”
The study was published in the Journal of Neural Engineering.