.jpg)
The director of the Wake Forest Institute for Regenerative Medicine and the W. Boyce professor and chair of Urology at Wake Forest University has been recognized by R&D Magazine for his advancements in the growth and regeneration of tissues and organs. (Credit: Wake Forest Institute for Regenerative Medicine)
Anthony Atala, M.D., is a pediatric surgeon by training. He often performs surgery on his youngest and most vulnerable patients. And it’s no easy task for him.
“There’s nothing more devastating than being in the operating room and doing surgery on patients where you’re putting things in that really don’t belong there, but you know that’s the only option you have. And you know that they’re prone to cause problems, but you don’t have a better option,” he told R&D Magazine in an exclusive interview.
This is why the director of the Wake Forest Institute for Regenerative Medicine (WFIRM) became a pioneer in growing and regenerating tissues and organs via 3D bioprinting. WFIRM is a leader in translating scientific discovery into clinical therapies. The institute’s scientists were the first in the world to successfully implant a laboratory-grown organ into humans in 1999—the bladder. His team has gone on to implant laboratory grown urethras and vaginas into patients. Ten technologies developed at the institute have been used clinically.
“Having engineered tissue that’s made out of a patient’s own cells—to replace tissue with tissue—that’s really the goal,” he said.
As organ shortages continue to be a national challenge and have been declared a public health crisis by the American Hospital Association, people are living longer and aging more, and therefore more organ failures occur. In fact, in a 10-year period, the number of patients on a transplant wait list doubled, while at the same time the actual number of organ transplants went up by less than 1 percent, according to Atala.
“The goal of regenerative medicine is to try to regenerate the patient’s tissues and organs,” Atala added. “And one strategy is to take a very small piece of tissue from the patient to extend the cells outside the body, create a new tissue or organ and then put it back into the patient; so that’s a lot of what we’ve been doing over several decades.”
What is 3D bioprinting?
3D bioprinting is the process of creating cell patterns in a confined space using 3D printing technologies where cell function and viability are preserved within the printed construct. Recent progress has allowed the 3D printing of biocompatible materials, cells and supporting components into complex 3D functional living tissues. The technology is being applied to regenerative medicine to address the need for tissues and organs suitable for transplantation.
Compared with non-biological printing, 3D bioprinting involves additional complexities, such as the choice of materials, cell types, growth and differentiation factors, and technical challenges related to the sensitivities of living cells and the construction of tissues.
How it all began
Atala and his team first started printing human organs about 14 years ago, when the world of bioprinting was still very new. They started out using desktop picture printers. And while these printers could create structures, the researchers quickly realized that those printers didn’t really have the structural integrity necessary to be implanted surgically in order to survive long-term. So three years later, the team started designing its own specialized printers, which used cells with gels instead of ink.
“The whole purpose of the printers was to be able to create human tissues and organs that you could print, and that they would have the structural integrity necessary to be planted surgically and also the ability to have the right blood vessels and nerves for them to function long-term,” Atala added.
The Atala team started out its bioprinting journey in the lab by first experimenting with the least complex organ structure—a flat one—such as skin. The tubular tissues, such as blood, are the second level of complexity. Following were the hollow, non-tubular organs, such as the bladder. And lastly, the most complex— the solid organs—such as the kidney and the heart were bioprinted as well.
Materials
As far as the material composition of the regenerative organs created, the Wake Forest team uses the patient’s own cells, taking a very small piece of the tissue from the patient and then extending those cells outside the body. For 3D bioprinting, the scientists used bio inks, also known as hydrogels that were designed to create the tissue. All of the materials that the Wake Forest team uses are compatible with the body. These materials are often used in surgery procedures, according to Atala.
“They’re nontoxic,” he said, “We design the bio inks with materials that have already been used clinically.”
3D bioprinting today and in the future
While 3D bioprinting is not yet being commercially applied to humans due to FDA regulatory issues, Atala and his team have already implanted several organs made by hand into humans, such as cartilage, bladders and urethras, which were approved by the FDA to go into clinical trials.
Currently, Atala and the Wake Forest team are focused on perfecting the printing technologies to prepare the organs that have already been printed and have risen to a satisfactory level, so they’re ready to be implanted into the body for mainstream use.
They are looking for ways to create insulin-producing cells in the laboratory, engineer blood vessels for heart bypass surgery and apply their regenerative medicine technologies to battlefield injuries through co-leading a federal grant, as well as many other novel research initiatives, according to the institute’s website.
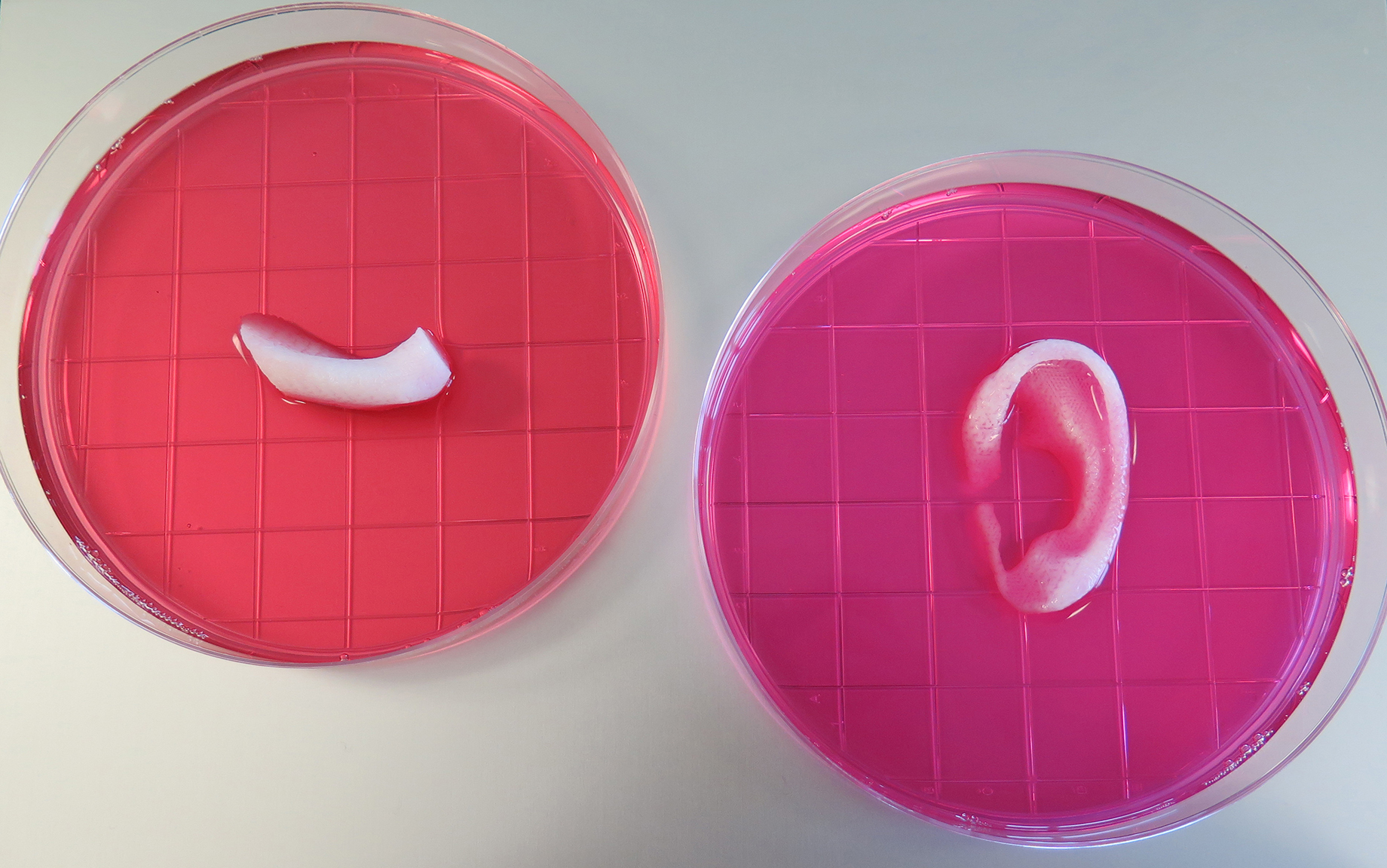
This photo shows a completed ear and jaw bone structures printed with the Integrated Tissue-Organ Printing System. (Credit: Wake Forest Institute for Regenerative Medicine)
Wounded Warrior Project
Speaking of battlefield injuries, Atala and the WFIRM have undertaken a great task on a national level—applying their expertise in regenerative medicine in a variety of projects to help wounded warriors. Atala and his team have been working for the past eight years on several federally funded research projects aimed at developing new treatments for military personnel. This national $75 million effort was started by the U.S. Department of Defense.
Through the Armed Forces Institute of Regenerative Medicine (AFIRM), a federally funded institution in the United States, teams of scientists are working to develop clinical therapies over the next five years that will focus on five areas: skin regeneration for burn injuries, restoring function to severely traumatized limbs, reconstruction for facial and skull injuries through tissue regeneration, new treatments to prevent rejection of “composite” transplants, such as face and hands, and reconstruction of the genital and urinary organs and lower abdomen. Atala attended the World Stem Cell Summit last month to speak about Wake Forest’s involvement in the Wounded Warrior Project.
In five to 10 years, the surgeon and researcher sees the technology of 3D bioprinting booming and going commercial. He has no doubt that there will be more instances of seeing tissues going into patients from 3D bioprinters, starting out with the least complex one, and moving on to more complex organs going forward.
The humble pioneer
Atala graduated from the University of Miami in 1984 and received his doctorate degree a year later at the University of Louisville. He did most of his training at the University of Louisville School of Medicine from 1985 through 1990. He also received his Pediatric Urologic Surgery Subspecialty training at Children’s Hospital and Harvard Medical School in Boston from 1990 to 1992. He is married with two sons.
The director of WFIRM has garnered several awards for changing people’s lives, including the U.S. Congress funded Christopher Columbus Foundation Award. He was also named by Scientific American as a Medical Treatments Leader of the Year. He is the editor of 10 books, serves on the editorial board of several journals, and has applied for or received more than 200 national and international patents.
Nevertheless, when asked what advice he would give upcoming generations of physicians and scientists in terms of focus in their careers to make an impact, his response was a very humble one.
“The goal, I think, is really to keep the patient at the forefront of everything you do,” he concluded. “In terms of the research direction, you have to start with the needs of the patient, and then move backwards. At the end of the day, we’re doing this to make the patients’ lives better and they are the heroes really.”