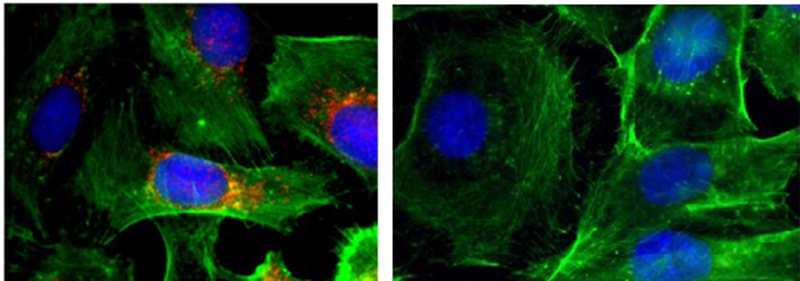
Immunofluorescence images of cells (nuclei shown in blue; actin shown in green; BRAF shown in red). Left: control; right: after treatment with nano- particles that silence BRAF.
Anaplastic thyroid cancer (ATC), the most aggressive form of thyroid cancer, has a mortality rate of nearly 100 percent and a median survival time of three to five months. One promising strategy for the treatment of these solid tumors and others is RNA interference (RNAi) nanotechnology, but delivering RNAi agents to the sites of tumors has proved challenging. Investigators at Brigham and Women’s Hospital, together with collaborators from Massachusetts General Hospital, have developed an innovative nanoplatform that allows them to effectively deliver RNAi agents to the sites of cancer and suppress tumor growth and reduce metastasis in preclinical models of ATC. Their results appear this week in The Proceedings of the National Academy of Sciences.
“We call this a ‘theranostic’ platform because it brings a therapy and a diagnostic together in one functional nanoparticle,” says co-senior author Jinjun Shi, PhD, assistant professor of Anesthesia in the Anesthesia Department. “We expect this study to pave the way for the development of theranostic platforms for image-guided RNAi delivery to advanced cancers.”
RNAi, the discovery of which won the Nobel Prize in Physiology or Medicine 10 years ago, allows researchers to silence mutated genes, including those upon which cancers depend to grow and survive and metastasize. Many ATCs depend upon mutations in the commonly mutated cancer gene BRAF. By delivering RNAi agents that specifically target and silence this mutated gene, the investigators hoped to stop both the growth and the spread of ATC, which often metastasizes to the lungs and other organs.
When RNAi is delivered on its own, it is usually broken down by enzymes or filtered out by the kidneys before it reaches tumor cells. Even when RNAi agents make it as far as the tumor, they are often unable to penetrate or are rejected by the cancer cells. To overcome these barriers, the investigators used nanoparticles to deliver the RNAi molecules to ATC tumors. In addition, they coupled the nanoparticles with a near-infrared fluorescent polymer, which allowed them to see where the nanoparticles accumulated in a mouse model of ATC.
By measuring the glow from the near-infrared fluorescent polymer, the team verified that nanoparticles had reached the primary site of ATC in the thyroid. The team found that the nanoparticles circulated for long periods of time in the blood stream and accumulated at high concentrations in the tumors.
In addition, the team reports evidence that BRAF had been successfully silenced at these sites. They found that, for cells grown in a dish and treated with the nanoparticles containing RNAi agents, cell growth was drastically slowed and the number of cancer cells that were able to migrate decreased by as much as 15-fold. In mouse models, tumor growth was also slowed and fewer metastases formed.
In order to translate the new platform into clinical applications, the research team notes the importance of having an imaging diagnostic that will allow them to quickly assess which patients most likely to benefit from RNAi nanotherapeutics.
“Most patients who present to surgeons with anaplastic thyroid cancer are out of options and this new research gives these patients some options. Having an approach that allows us to rapidly visualize and simultaneously deliver a targeted therapy could be critical for the efficient treatment of this disease and other lethal cancers with a poor prognosis,” says co-senior author, Sareh Parangi, MD, associate professor in the MGH Department of Surgery.
This work was supported by the NIH grants R00CA160350, CA200900, CA149738, EB015419, and U54-CA151884; by the DoD PCRP Synergistic Idea Development Award; by the Koch-Prostate Cancer Foundation (PCF) Program in Nanotherapeutics, Movember-PCF Challenge Award and PCF Young Investigator Award; and by the National Research Foundation of Korea K1A1A2048701.
Source: Brigham and Women’s Hospital




