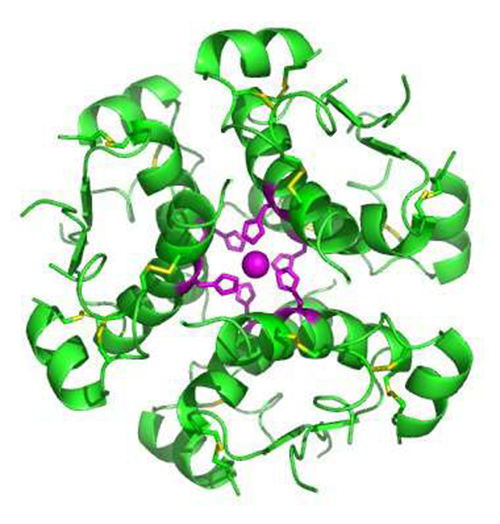
High-resolution model of six insulin molecules assembled in a hexamer. (Credit: Isaac Yonemoto/Wikipedia)
New Zealand researchers have uncovered a new mechanism that controls the release of the hormone insulin in the body, providing hope for those with a genetic susceptibility to type 2 diabetes.
The findings, published today in the Journal of Biological Chemistry, show for the first time that a protein known as beta catenin is crucial for controlling the release of insulin from the pancreas to maintain stable blood sugar levels.
In type 2 diabetes, either the body doesn’t produce enough insulin or the cells in the body don’t recognise the insulin that is present, leading to high levels of glucose in the blood.
University of Auckland lead researcher Prof. Peter Shepherd and his team, including Brie Sorrenson, Ph.D., carried out the study with the support of a $1.2 million project grant from the Health Research Council of New Zealand (HRC).
For this part of the project they focused on a variant in a gene called TCF7L2. This variant has been known to science for about 10 years and is the biggest contributing factor for whether people are genetically susceptible to getting type 2 diabetes or not.
“We wanted to understand what happens in the body’s cells that are associated with TCF7L2 and how the processes that go on affect the regulation of glucose metabolism in the body,” said Shepherd.
“TCF7L2 binds directly to beta catenin. By observing this interaction, we found that beta catenin levels not only change in response to rising and falling nutrient levels, but that they also regulate how much insulin we have in our body and ensure that we have the right amount of insulin at the right time.”
“Scientists have built up a large body of knowledge over the past 15 years about how hormones are released from cells in the body, but this is the first time this mechanism has been associated with the release of insulin,” said Shepherd.
“One possible reason for this delay is that beta catenin has in the past been closely associated with cancer, not diabetes.
“Underneath the cell membrane there are layers of fibres called actin. These fibres form networks that somehow bind to insulin,” he added.
“Our evidence suggests that beta catenin is controlling these networks of actin fibres and rapidly changing their nature by opening up ‘gaps’ in the fibre network to either block or allow the release of insulin.”
Although this paper focuses specifically on type 2 diabetes, the team’s preliminary findings as part of the wider HRC-funded project suggest that the same mechanism also helps control the way insulin functions; the metabolism of glucose in fat cells; and the release of hormones in the brain that control appetite and energy metabolism.
“We think we’ve identified a much broader mechanism that affects multiple cell types, not just beta cells in our pancreas,” said Shepherd.
HRC Chief Executive Professor Kath McPherson says we can’t develop new treatments for chronic diseases like diabetes, unless we understand the biology behind them and this is one of the reasons why fundamental scientific research like this is so important.
“Peter and his team have received significant HRC funding over the years to pursue this avenue of research,” she said.
“Major outcomes like this highlight the benefits of long-term HRC funding for emerging science in New Zealand. It’s hard work finding new mechanisms that contribute to disease – researchers must go down a lot of blind alleys to find them.
“There’s a very high payoff in the end in terms of enhancing our understanding of disease and developing potential new treatments,” said McPherson.
Between 50 and 60 per cent of people who are susceptible to type 2 diabetes in our current environment have a genetic variant that puts them at higher risk of getting the disease.
“This discovery potentially opens up a whole new drug discovery field to understand how we could manipulate beta catenin levels to control the release of insulin,” concluded Shepherd.



