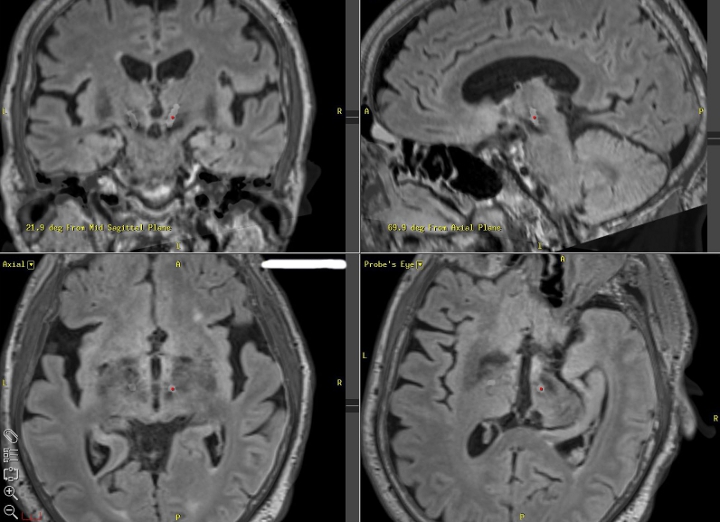
An MR image of the brain from Duke University. (Credit: Duke University)
A new method to narrow down more effective patterns of electric shock could lead to personalized treatment options for patients suffering from Parkinson’s disease.
Biomedical engineers from Duke University have begun treating Parkinson’s disease symptoms by using computers to evolve more effective patterns of electric shocks delivered deep within the brain.
The new strategy could reduce the number of battery replacement surgeries needed during a patient’s lifetime and lead to patterns tailored to treat the specific symptoms of the degenerative disorder.
Deep brain stimulation which sends electrical pulses deep into the brains of people suffering from neurological motor control diseases through wires implanted into an area of the brain called the basal ganglia was first introduced in 1987.
While the reasons remain unclear, stimulation has shown to greatly improve motor functions in many patients.
However, through further analysis Duke engineers discovered that timing patterns of deep brain stimulation became less effective as they became random, leading credence to the theory that Parkinson’s treatment can be individualized.
The implication that there might be non-random patterns that work better than a constant barrage of pulses to treat the disease led Duke researchers to build an evolutionary computer algorithm to more purposefully design effective patterns.
The program developed a pattern that cuts stimulator energy usage by up to 75 percent while losing none of the treatment’s benefits.
Warren Grill, Ph.D., the Edmund T. Pratt Jr. School professor of Biomedical Engineering, said the new treatment method can be more effective while also saving money and energy.
“Cutting energy use is important because when these devices’ primary cell batteries run out, they have to be replaced through a surgical procedure,” Grill said in a statement. “Besides being expensive, studies have shown that that there is a 2 to 3 percent chance of infection, which goes up each time the procedure is done.
“And because these batteries only last three to five years, someone receiving an implant at age 50 could undergo many procedures in a lifetime.”
The researchers were able to develop timing patterns by splitting each second of electrical pulses into five segments, which they then divided into 200 individual slices. Each segment formed one repetition of a pattern, with each millisecond-long slice randomly receiving a pulse or a blank. However, doing this resulted in 100 quindecillion possible patterns, rendering it virtually impossible to pick the promising patterns.
“The method works very similarly to biological evolution but it occurs inside of a computer,” Grill said. “In our world, instead of a giraffe’s neck getting longer to reach higher leaves, the positions of electric pulses change so that the pattern gets better over time.”
The algorithm randomly creates 10 patterns of deep brain stimulation and tests them in a computational model of Parkinson’s disease.
The better patterns then “parent” a new pattern and in each generation the computer introduces random mutations into the offspring as well as new “immigrant” patterns to keep the gene pool fresh.
After testing thousands of iterations, a new, highly efficient pattern is chosen.
The algorithm evaluated the patterns based on efficiency and effectiveness and by weighting the two appropriately, the computer evolved patterns that used the least amount of energy while maintaining performance just as good as a standard, constant stream of pulses.
Another benefit is the pattern that emerged used only about 45 pulses per second, while the industry standard is currently between 130 and 185 pulses per second—an energy savings of 60 to 75 percent, which could double or triple the lifetime of the implanted battery.
Grill’s team originally tested the algorithm on rats and after promising results they moved on to human patients. Grill and his team collaborated with neurosurgeons at Duke Health and Emory Healthcare in Atlanta in recruiting patients with deep brain stimulation implants to test the pattern when they came in for surgical battery replacements. These patients only received local anesthesia during the surgical procedure, retaining control over many motor functions so researchers could assess their symptoms.
In between the removal and installation of batteries the patients were temporarily connected to the test devices and the computationally evolved pattern performed just as well as the individually optimized treatments developed by each patient’s neurologist over the course of many years, while requiring substantially less energy.
The study appeared in Science Translational Medicine.

Two implantable pulse generators used for deep brain stimulation. The energy savings from the novel temporal pattern of stimulation can either make the battery last longer or allow for a much smaller implantable device. (Credit: Duke University)