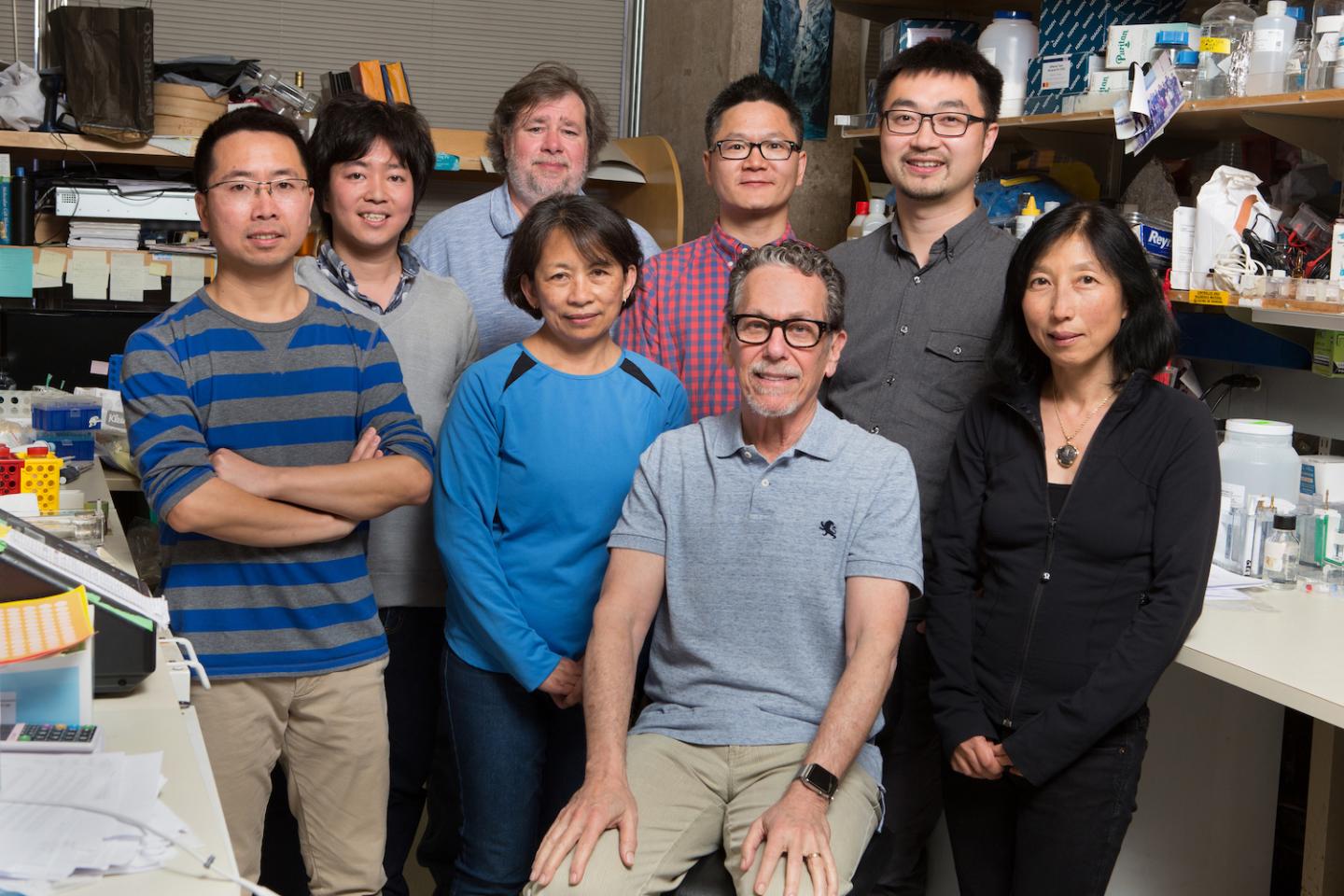
From left: (front row) Nanhai He, Gabriela Estepa, Ron Evans and Ruth Yu; (back row) Eiji Yoshihara, Michael Downes, Weiwei Fan and Zong Wei.
More than 27 million people in the United States are living with type 2 diabetes, according to the Centers for Disease Control and Prevention. As the population ages and a growing percentage of people become overweight or obese, that number is expected to increase.
In a paper published May 10, 2018, in Cell, researchers from the Salk Institute report a potential new approach for treating diabetes by protecting beta cells–the cells in the pancreas that produce, store and release the hormone insulin. When beta cells become dysfunctional, the body can’t make insulin to control blood sugar (glucose) and levels of glucose can rise to dangerous–even fatal–levels.
The investigators accomplished their goal by using an unexpected source: vitamin D. Vitamin D in cells and mouse models proved beneficial in treating damaged beta cells. It also provided new insights about gene regulation that could be applied to developing treatments for other diseases, including cancer.
“We know that diabetes is a disease caused by inflammation,” explains senior author Ronald Evans, a Howard Hughes Medical Institute investigator and holder of Salk’s March of Dimes Chair in Molecular and Developmental Biology. “In this study, we identified the vitamin D receptor as an important modulator of both inflammation and beta cell survival.”
Using beta cells created from embryonic stem cells, the investigators were able to identify a compound, iBRD9, that appeared to enhance the activation of the vitamin D receptor when it was combined with vitamin D to improve the survival of beta cells. The team accomplished this by conducting a screening test to look for compounds that improved the survival of beta cells in a dish. They then tested the combination in a mouse model of diabetes and showed that it could bring glucose back to normal levels in the animals.
“This study started out by looking at the role of vitamin D in beta cells,” says Zong Wei, a research associate in Salk’s Gene Expression Laboratory and the study’s first author. “Epidemiological studies in patients have suggested a correlation between high vitamin D concentrations in the blood and a lower risk of diabetes, but the underlying mechanism was not well understood. It’s been hard to protect beta cells with the vitamin alone. We now have some ideas about how we might be able to take advantage of this connection.”
The underlying process has to do with transcription–the way that genes are translated into proteins. Combining the new compound with vitamin D allowed certain protective genes to be expressed at much higher levels than they are in diseased cells.
“Activating the vitamin D receptor can trigger the anti-inflammatory function of genes to help cells survive under stressed conditions,” says Michael Downes, a Salk senior staff scientist and co-corresponding author. “By using a screening system that we developed in the lab, we’ve been able to identify an important piece of that puzzle that allows for super-activation of the Vitamin D pathway.”
The discovery’s implications can have far-reaching implications: It identifies a basic mechanism that can be translated into drugging many different targets in the clinic.
“In this study, we looked at diabetes, but because this is an important receptor it could potentially be universal for any treatments where you need to boost the effect of vitamin D,” adds Ruth Yu, a Salk staff researcher and one of the study’s authors. “For example, we are especially interested in looking at it in pancreatic cancer, which is a disease that our lab already studies.”
The investigators say that, although the new compound did not appear to cause any side effects in the mice, further testing is needed before clinical trials can begin.




