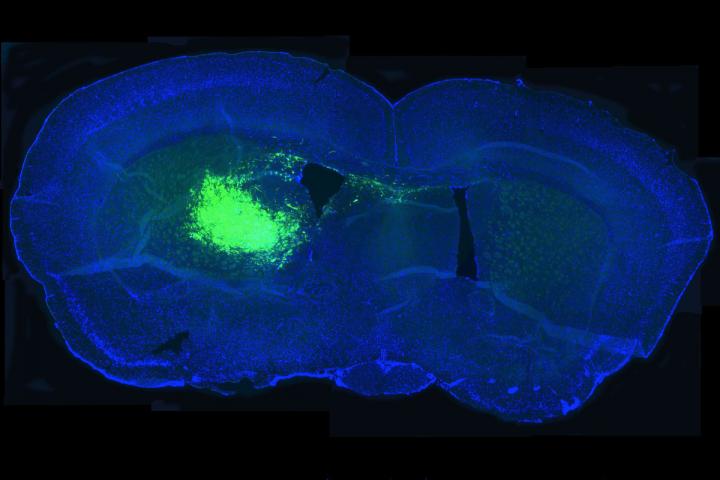
Researchers have shown that a metabolic pathway associated with slowing aging also drives brain cancer. In this image, cancer stem cells in a mouse brain section glow fluorescent green, allowing researchers to study the effect of inhibiting the pathway on the ability of cancer stem cells to survive and proliferate. Source: Amit Gujar and Albert H. Kim
While a particular metabolic pathway shows potential to slow down the aging process, new research indicates a downside: That same pathway may drive brain cancer.
The pathway, known as the nicotinamide adenine dinucleotide (NAD+) pathway, is overactive in a deadly form of brain cancer known as glioblastoma, according to a study by researchers at Washington University School of Medicine in St. Louis. Glioblastoma is the most common and aggressive brain cancer in adults. Over 70 percent of patients with glioblastoma die within two years of diagnosis.
The new research showed that glioblastoma patients with high expression of an NAD+ pathway gene known as NAMPT died sooner. Tumors with elevated expression of the same gene grew rapidly when they were implanted in mice and shrank when NAMPT was inhibited.
The study, published Dec. 5 in Proceedings of the National Academy of Sciences, suggests that inhibiting the NAD+ pathway may improve the outlook for glioblastoma patients but also may affect other biological processes, such as aging.
NAMPT produces a molecule known as nicotinamide mononucleotide (NMN) that has been shown to reduce signs of aging in mice. While its safety in people has yet to be determined – a clinical trial is ongoing in Japan – NMN and other molecules along the NAD+ pathway are being marketed as anti-aging supplements.
“There’s a lot of buzz about taking NAD+ precursors for their anti-aging effects, which is based on a lot of great science,” said Albert H. Kim, MD, PhD, an assistant professor of neurological surgery and the senior author on the study. “We didn’t directly demonstrate that taking NAD+ precursors makes tumors grow faster, but one implication of our work is that if you want to take anti-aging NAD+ precursors, you might want to keep in mind that we don’t yet understand all the risks.”
Using human glioblastoma cells, Kim, postdoctoral researcher Amit Gujar, PhD, and colleagues showed that NAMPT helped cancerous stem cells survive and proliferate, fueling the growth of existing tumors, while inhibiting NAMPT reduced the ability of the cancer stem cells to renew themselves.
Furthermore, the scientists found that glioblastoma cells responded to radiation therapy – a standard therapy used to treat the disease in people – by increasing expression of NAD+ pathway genes, and that inhibiting NAMPT before dosing the cells with radiation made them easier to kill.
“If you target the NAD+ pathway, you can disrupt the ability of the cancer stem cells to self-renew, and you can also make them more sensitive to radiation treatment,” said Kim, who also treats patients with brain tumors at Siteman Cancer Center at Washington University School of Medicine and Barnes-Jewish Hospital. “In a patient, that could mean that if you suppress the pathway, the same dose of radiation may be more effective at destroying the tumor.”
The NAD+ pathway involves many different genes and proteins, and its very complexity may be the key to having it both ways. Kim believes it may be possible to carefully modulate the pathway so as to suppress cancer without accelerating aging or interfering with other important biological processes.
“The question we are considering now is, ‘How do we make an NAD+ strategy that is specific for cancer?'” Kim said. “Maybe there are some cancer-specific regulators, and we can disrupt those. Maybe we can change the expression of some key NAD+ pathway genes only in cancer cells, not healthy cells. There are many ways to look at this, and that’s why we want to dig deeper into how this pathway works in glioblastoma.”




