The R&D 100 Awards and Conference
Bette Korber, PhD, will receive her 2018 Scientist of the Year Award at the 2018 R&D 100 Award’s black-tie ceremony on Nov. 16, 2018, at the Waldorf Astoria Orlando. This year marks the 53nd annual Scientist of the Year Award, which recognizes career accomplishments in scientific research and technology spanning nearly all disciplines. The same event will also recognize the 2018 R&D 100 Award winners.
The R&D 100 Awards have served as the most prestigious innovation awards program for the past 55 years, honoring great R&D pioneers and their revolutionary ideas in science and technology. The R&D 100 Awards will take place following the fourth annual R&D 100 Conference, Nov. 15-16, 2018. At this year’s event leaders from the R&D community will gather to exchange brand-new ideas in innovation, technology transfer and R&D strategies that will transform the future of R&D across industries. Together, the R&D 100 Awards presentation event and the R&D 100 Conference offer an enriching, one-of-a-kind experience for R&D professionals of all levels and specialties.
For more information visit https://www. rd100conference.com
Applications for the 2019 R&D 100 Awards are now being accepted. Go to www.rd100conference.com/awards to apply.
Bette Korber, PhD, has certainly had an impressive career.
Since joining Los Alamos National Laboratory (LANL) in 1991 she has managed and build up the lab’s HIV Database and Analysis Project, which today features over 840,000 sequences of the HIV virus from around the world.
Utilizing that same database, she then built an innovative vaccine design known as “mosaic,” created to overcome the extreme diversity of the HIV virus. It combines sets of proteins—assembled from fragments of natural sequences via a computational optimization method— to maximize vaccine coverage in the most efficient way possible.
Today, her mosaic design is the key element of a first-in-class preventative HIV vaccine now being tested for efficacy in humans in a Phase II clinical trial, a milestone few HIV vaccines have reached.
Despite these achievements, Korber—R&D Magazine’s 2018 Scientist of the Year—has not had an especially easy path to success.
In the 1980s during her time as an undergraduate at California State University, Long Beach and as a graduate student at the California Institute of Technology (Caltech), Korber was discouraged from following her passion for computational biology.
“As an undergraduate my skills were more in programing and math, but I kind of got pushed into the direction of experimental biology, I think because I was a woman at that time,” said Korber, in an exclusive interview with R&D Magazine. “Mentors pushed me in that direction, but I always really wanted to do computational work.”
Despite her interest, ultimately, Korber—one of only a handful of women at Caltech at the time—listened to her mentors and focused on bench work, receiving her PhD in immunology and chemistry in 1988.
Looking back she regrets letting others discourage her from her true passion and hopes that women today who are interested in male-dominated fields don’t make the same mistake.
“I was shy and young and in a man’s world and I didn’t stand up for myself,” she said. “Although I don’t think what happened to me happens as often now, women still need to encourage each other and men need to take women seriously, not just brush off their ideas, or worse, take their ideas, which still happens all the time. We have to fight back, we have to stand up for ourselves and each other.”

Bette Korber, PhD, Credit: Bette Korber
Finding her path
Although she started on a different path than she initially intended, Korber’s early work in immunology ended up shaping the trajectory of her career. During the time she was working on her PhD and studying the intricacies of the immune system, her close friend and roommate became one of the earliest people to be diagnosed with HIV.
“I was a basic immunologist working on mouse immunology like everyone does, but because of him contracting HIV and there being absolutely no way to cure it at that time, I got very interested in it,” explained Korber. “When I did a post-doc at Harvard I started working in the HIV field.”
Following her post-doc, Korber—along with her husband, fellow Caltech alumni and scientist James Theiler, PhD—moved to New Mexico and joined LANL in 1991. It was there that she was truly able to combine her interest fighting HIV with her passion for computing.
She quickly connected with Gerry Myers, PhD, the LANL researcher who had founded the lab’s HIV Database—the first-ever pathogen database—which at the time had just a few hundred sequences.
“I was really excited when I got the opportunity to come to Los Alamos and sort of leave bench work behind and sit full-time at the computer,” said Korber. “Gerry was really open to letting me re-learn and re-awaken the kinds of skills that I was more interested in, which were more analytical skills.”
Myers—who passed away in 2011—started the HIV Database in 1986 with the goal to collect, curate, and annotate HIV genetic material, and then provide the data to scientists in an open-access environment to encourage collaboration within the field. The initial data came from an earlier LANL effort called GenBank, a public database set up in 1982 to store laboratory samples of previously sequenced organisms.
Shortly after Korber began working with Myers she founded the sister HIV Molecular Immunology Database, the first immunology database. The two databases were then coupled, giving the researchers the ability to study the relationship between an immune response and the HIV sequences.
“It’s an integrated database where we pull together the HIV immunology data and all the HIV sequence data, and we make computational tools to go between the two of them,” said Korber. “I think there are other immunology databases now and there are other pathogen databases now, but this is still kind of unique with the cross fertilization that it has.”
The database—which quickly expanded—became the basis for Korber’s research.
“When Gerry and I were first working on it had just a few hundred sequences and then we got a few hundred more and then thousands,” said Korber.
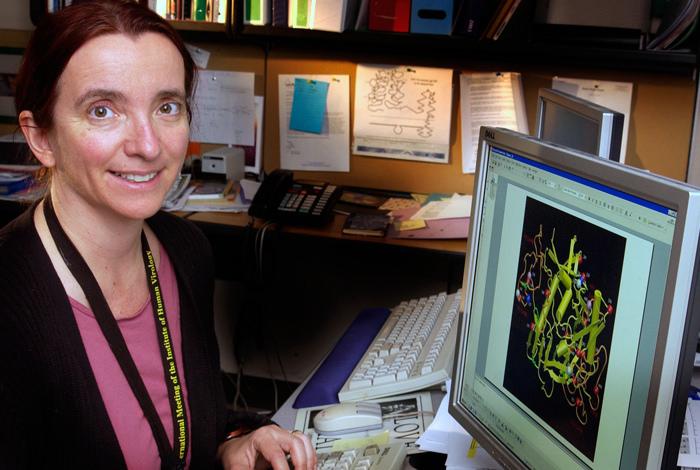
At Los Alamos National Laboratory, Bette Korber founded the first immunology database, known as the HIV Molecular Immunology Database. Credit: Los Alamos National Laboratory
A novel approach
As the database grew, so did its ability to inform Korber’s research. It was through the database that she first began to understand the potential of a mosaic vaccine design in the early 2000s.
“My vaccine work grew out of gathering all of that global data and feeding it back to the community, and then having my own research be part of using that global data,” explained Korber.
Looking at the data, Korber also began to understand why other HIV vaccines had failed.
“HIV is incredibly variable, and I think that is the main reason we haven’t had a working vaccine to date,” she said. “It evolves differently in every single infected person during the course of his or her infection. It evolves in different ways; not just by base mutation but by insertion and deletion, recombination, glycosylation patterns can change. It’s just extraordinarily variable.”
Typically, vaccines are designed to stimulate an immune response using one antigen or virus that is specifically targeted. However, because HIV is so variable between different individuals, the immune response the vaccine triggers must be able to interact with many different viruses.
Korber and her team worked to design the database to identity epitopes—bits of the virus that the immune system can recognize—and evaluate the evidence for the strength of each epitope. Through this work, Korber discovered that HIV is packed with epitopes, a finding that directly led to the creation of the mosaic vaccine approach.
“The mosaic was inspired by pulling together the database and just looking at the variability virtually every day and looking at how densely packed it was with little bits that the immune system could see; it was just that you’ve got to get an immune response that is cross reactive and see all the variance,” said Korber.
To achieve this, Korber and her team looked at virus sequences from all over the world, and using computer optimization, determined which few sequences would provide the optimal coverage of global HIV viruses. The computer then created synthetic antigens that are approximations of those sequences.
“What the mosaic does is it evolves sequences in a computer to solve a problem on how to—with just a couple of sequences—give the best immunological coverage you can,” explained Korber. “Instead of putting in two natural strains, you make two computationally designed strains that are kind of central and complement one another to really get the best coverage you can with just a couple of strains.”
Because no natural proteins were involved in this approach—contrary to typical vaccine design—Korber’s idea was not initially well received. In fact, she was denied for several of the first grants she applied for.
“There was extreme pushback, no one thought it had a chance,” she said. “These were constructed proteins that were evolved on a computer. People just didn’t think that they would fold, that they would make good immune responses, that they would be stable. But I followed the principles of the way that HIV evolved. Even after we showed that people still remained skeptical that it would work. It takes a little while for a field to get used to an idea.”
Eventually, she was able to secure funding to pay for the computational support she needed to create the mosaic via an internal LANL grant. She then reached out to several experimentalist colleagues to help with the project, including Barton Haynes, MD from Duke University and Dan Barouch, MD, PhD from Harvard University.
The project became a multidisciplinary endeavor with Korber and her LANL colleagues determining the design of the mosaic using computing techniques, and Haynes and Barouch building the synthetic antigens in their laboratories and testing them on small animals. She also recruited computational experts including now former LANL scientist Simon Perkins, PhD who wrote much of the mosaic codes for the vaccine. Korber’s husband Theiler, a mathematician and physicist, also collaborated with her on the project.
“The interdisciplinary aspect is really what made it fly,” said Korber. “I couldn’t have coded something this deep without Simon, but he could not have framed the question or figured out what to code without me working with him.”
The team published their first paper on the concept in 2007, a challenge in itself among a scientific community that still had its doubts about what they were doing.
“When you have an idea for designing a protein that is very different than anyone has tried before, selling that is very difficult,” said Korber. “It was very challenging trying to convince someone that this actually could work.”

Bette Korber presenting her work at a recent meeting. Credit: Bette Korber
Seeing results
It was Barouch—who serves as a professor of medicine at Harvard Medical School and the director of Center for Virology and Vaccine Research at Harvard—who helped Korber move her concept into the clinic. He designed a vaccine that used a strain of a common-cold virus— engineered so that it does not cause illness— to deliver the mosaic antigens Korber had computationally designed.
The vaccine was first tested on monkeys, where it showed promise.
“We found that, indeed, these proteins that we had designed were stable and they were really immunogenic,” said Korber. “When they were put into monkeys, the monkeys made really good immune responses and the immune responses that the monkeys made tended to be more cross reactive. They did what we wanted them to do in vaccinated animals.”
Preclinical studies with the mosaic-based vaccine regimen confirmed this, demonstrating that they were effective in protecting monkeys against infection with an HIV-like virus. Then two early-stage human clinical trials suggested that these vaccines are well-tolerated and can generate anti-HIV immune responses in healthy adult volunteers.
As a result, the National Institutes of Health (NIH) launched a large clinical trial in November 2017 to assess whether the mosaic HIV vaccine regimen is safe and able to prevent HIV infection in humans. The study is sponsored by Janssen Vaccines & Prevention, B.V., part of the Janssen Pharmaceutical Companies of Johnson & Johnson, with co-funding from two primary partners, the Bill & Melinda Gates Foundation and NIH’s National Institute of Allergy and Infectious Diseases. The new Phase IIb proof-of-concept study, called Imbokodo, aims to enroll 2,600 HIV-negative women in sub-Saharan Africa. The first Imbokodo participants received vaccinations at clinical research sites in South Africa, followed by participants in Malawi, Mozambique, Zambia, and Zimbabwe. Participants will be followed for at least two years.
Although Korber herself has stepped away from the clinical trial portion of this research, she is still closely watching its progress. She serves as an advisor for the project for both Barouch and Janseen.
“It is really exciting for me to know that this is getting taken forward and getting to witness it and helping out a little bit with the thinking, as the standard statistician doesn’t always think about sequence variation and all of that. I am glad I am able to help from that point of view,” said Korber.
Looking ahead
Although this particular HIV mosaic vaccine is the innovation Korber has that is furthest along in the pipeline, it is far from her only project.
She continues to work mainly in HIV vaccine optimization, focusing on approaches both related and unrelated to the mosaic concept. She has been working a mosaic vaccine that focuses just on conserved regions with colleagues at Oxford. Over the past few years, she has published papers on a second-generation algorithm she designed in collaboration with her husband called an Epigraph. This is an efficient graph-based algorithm for designing vaccine antigens to optimize potential epitope coverage (an epitope is a small part of a pathogen protein that the immune system can see). Epigraph vaccine antigens are functionally similar to mosaic vaccines, but in contrast to the mosaic algorithm, the epigraph code is much faster, and in some cases, provides a mathematically optimal solution.
In addition, Korber is working with experimentalist colleagues at Duke and Harvard on two other projects that they have not yet published research on. One is called a Signature-informed Epitope Targeting, or SET vaccine.
“It’s an idea where you look at the evolution of the viruses, and how that impacts how sensitive viruses are to antibodies, and then you design vaccines based on antibody activity and resistance patterns,” said Korber. “It is a quite different approach where you use a statistical measure to study the impact of diversity on antibody sensitivity, and to design vaccines. SET vaccines have shown some promise in guinea pigs so far, but we haven’t taken it further than that.”
Another approach she is working on, known as “structural mosaic,” takes into account the three-dimensional structure of a viral protein, as well as the sequence of the protein, explained Korber. This approach is also currently being tested in guinea pigs. Both strategies have yet to be tested for protection from infection, but Korber is optimistic about their potential.
Korber doesn’t know if the mosaic vaccine that is being tested in the Imbokodo trial— or any of her other ongoing projects— will result in a successful HIV vaccine, but she is hopeful either way. For Korber, even a failed idea is a worthwhile experience.
“If it does work that is wonderful, especially if it works to a level where it is actually useful enough to make it as a product,” said Korber. “If this doesn’t work we will learn from the trial anyway and we will learn why it didn’t work, maybe, and be able to do better the next trial. And meanwhile, both my laboratory and my colleague’s laboratories have other horses in the race. Either way it’s exciting.”